Pelvic Organ Prolapse: What you need to know.
Have you ever felt the sensation of vaginal heaviness or bulging or just ‘something there’?
Are you finding that you aren’t quite emptying completely from the bladder or bowel?
Or did your GP mention at your last pap smear that you have a prolapse?
Prolapse is a common issue with 5-10% of the female population reporting a sensation of something coming down/bulging into the vagina. However, based on clinical examination, POP can be observed in up to 41-54% of women although not all women are troubled by symptoms.
Read on to find out more about POP.
What is prolapse?
Prolapse means slipping or descent of a part of an organ.
Pelvic Organ Prolapse (POP) therefore refers to the downward movement of any of the pelvic organs, which include the uterus, bladder, urethra, rectum or bowel, into the vaginal space. The descent of pelvic organs can result from over-stretched or damaged ligaments, connective tissue and/or pelvic floor muscles.
This downward movement can happen in varying degrees and prolapses are graded from Stages 1 to 4. Stage 1 and some stage 2 prolapses you may not feel, but usually women with stage 2-4 prolapses are symptomatic.
More specific terminology includes:
• Cystocele: prolapse of the bladder
• Urethrocele: prolapse of the urethra
• Uterine prolapse or descent: prolapse of the uterus
• Vaginal vault prolapse: prolapse of the vagina (in women who have had a hysterectomy)
• Rectocele: prolapse of the rectum
• Enterocele: prolapse of the small bowel
What are the signs and symptoms of prolapse?
Some women with prolapse can experience symptoms including:
• A sensation of vaginal bulging
• A sensation of a lump or ‘something coming down’
• Pelvic pressure
• Abdominal heaviness or dragging sensation
• Low back ache
• Incomplete bladder or bowel emptying
• Pain or discomfort with intercourse or the sensation of an obstruction
Other signs of POP are:
• Feeling a protrusion vaginally on washing or wiping
• Urinary or faecal leakage
• Needing to support the perineum or splint vaginally to empty the bowels
• Symptoms can often feel worse at the end of the day, after a prolonged time on your feet or during/after lifting.
What can cause POP?
The development of POP is multi-factorial and due to a combination of environmental and genetic risk factors but generally activities that involve excessive straining and high intra-abdominal pressures can contribute to POP.
Risk factors include:
• Increasing parity (number of children delivered)
• Vaginal delivery especially instrumental delivery (eg. forceps)
• Damaged levator ani (pelvic floor) muscle
• Advancing age – time wounds all heels!
• Obesity/ increased body mass index (BMI)
• Constipation
• Chronic pelvic floor stress, labour intensive occupations such as repeated heavy lifting
• Genetic factors and differences in collagen and connective tissue types
• Nerve injury
• Previous hysterectomy and/or pelvic reconstructive surgery
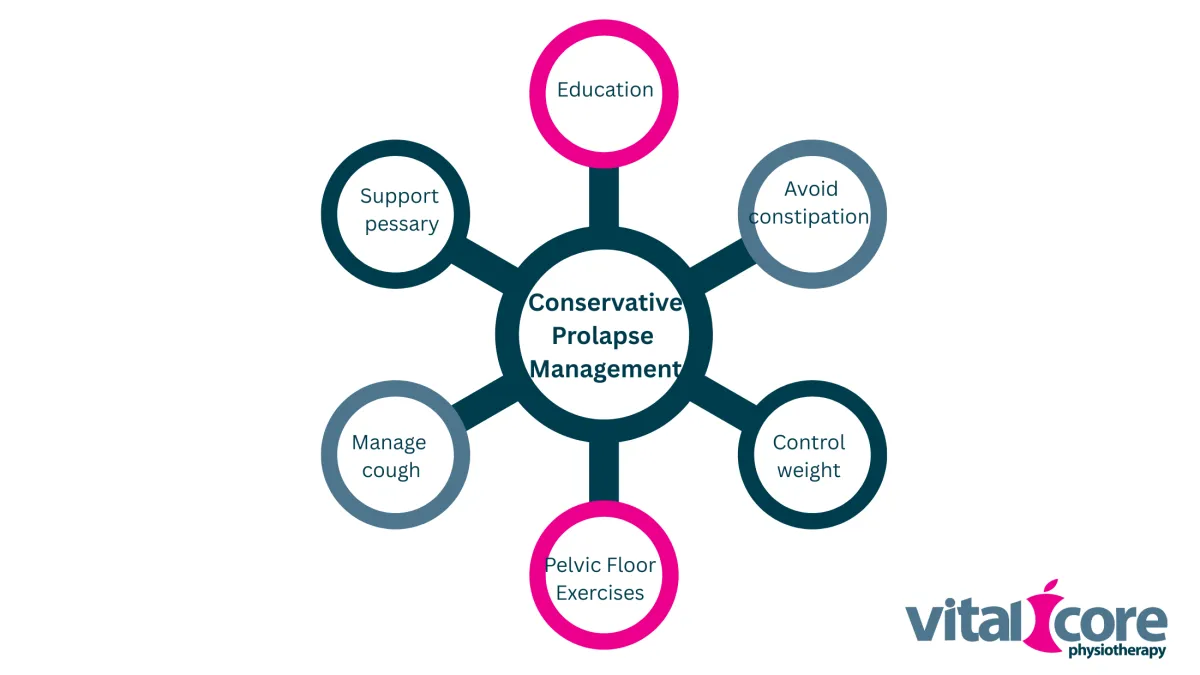
Can I do anything to help my prolapse?
There will be risk factors that you cannot change, like your age or having had children. However, based on research, you may minimise POP or prevent it worsening by:
• Avoiding constipation and straining
• Minimising weight gain and maintaining a healthy weight
• Doing regular pelvic floor exercises to maintain excellent strength and coordination of the pelvic floor muscles
• Managing any chest disease that can cause chronic cough and subsequent increases in intra-abdominal pressure
As symptoms can often feel worse after a while on your feet or after lifting, you should also aim to pace your physical activities, incorporate rest periods in sitting or lying, and seek help for heavier physical tasks if possible.
Learning how to activate your deep abdominal muscles and your pelvic floor muscles, and learning to breathe correctly may help to limit excessive increases in intra-abdominal pressure with lifting tasks and exercise.
What are the management options for POP?
Conservative management options include pelvic floor muscle (PFM) exercises and physiotherapy, and/or use of a vaginal pessary.
PFM exercises and Physiotherapy
The aim of PFM training is to increase the strength and bulk of the PFMs to help support the pelvic organs. PFM training has been shown to improve POP stage/severity and POP- associated symptoms, and is particularly beneficial with an individualised program and under supervision, which a physiotherapist can help you with. One of the most significant problems we see however is coordination of these muscles, and having them activate at the right time, with the right intensity of contraction. Again, this is where your pelvic health physio is your Pelvic PT!
Vaginal pessary
Pessaries are silicone devices that come in a variety of shapes and sizes and are inserted vaginally to help splint the vaginal walls and support the pelvic organs. Your pelvic health physiotherapist will examine your pelvic floor to fit you with the correct size and style of
pessary, and they will also teach you how to self-manage your pessary if it’s appropriate.
Some pessaries can stay in for months at a time and others need to be taken out and cleaned daily. With good hygiene and regular follow-up with your physiotherapist, a vaginal pessary can offer excellent long-term symptom relief.
Surgical management
Surgery may be indicated for women with severe prolapse or symptomatic prolapse where conservative management has failed. Your Gynaecologist will be able to explain the different surgeries for POP. It should be noted that for 1 in 3 women, there can be a recurrence of POP post-surgery. Women undergoing surgery should therefore undergo PFM training before and after to help strengthen the muscles as best as possible.
I think I might have a prolapse – what should I do?
Book in for a pelvic floor assessment with one of Vital Core Physio’s post-graduate trained Physiotherapists with a special interest in prolapse management. They will be able to assess whether you have a prolapse and give you an individualised PFM training program and advice, as well as guide you with getting back into exercises and activities that you love. Your physiotherapist may also use real-time ultrasound to give you visual feedback about your PFM and deep abdominal activation.
Ask a question of Vital Core Physiotherapy
Fill in the form to request a Call From Our Team
One of our team will call you for FREE and answer any questions or concerns you may have about your condition
© 2023 Vital Core Physiotherapy